“Are you a smoker?”
“Yes”
“Have you ever thought about stopping?”
“No. I mean, I know I should.”
This is an all too familiar conversation. But how should we be responding? Should we take a hard line with regard to smoking in the perioperative period? Would it make a difference?
This month is Stoptober, a Public Health England campaign aimed at promoting smoking cessation services offered by the NHS. Coinciding with this, here at Concentric we wanted to understand how smoking impacts our patients’ perioperative risk, and what this means when discussing outcomes from surgery.
Smoking carries significant health risks. We know this. Our patients know this. Yet, despite public campaigns, advertising restrictions and raising the legal age to purchase cigarettes, 14.7% of the UK adult population are smokers. That’s 7.2 million people.
Smoking and surgery. So what?
Alongside others, The Royal College of Anaesthetists and the NHS have published information for patients and healthcare professionals on the impacts of smoking around the time of surgery. There is a body of evidence, developed over a number of decades, describing a list of preventable complications that come with preoperative smoking.
A significant contributor to this body of evidence is a large study from the American College of Surgeons’ National Surgical Quality Improvement Program (NSQIP) database which showed that smoking significantly increased the risk of postoperative pneumonia, cardiac arrest, myocardial infarction, stroke, wound infection, septic shock and requirement for intensive care. Most shockingly, it found that for patients undergoing non-cardiac surgery, smokers were 38% more likely to die after their operation.
So there’s a wealth of information available on this topic, and most of it doesn’t come as a surprise. But a crucial question is, are patients aware of the increased risks? Perhaps surprisingly, a recent Canadian survey showed that only half of patients were aware that continuing to smoke would increase their surgical risks.
What should our approach be to have a positive impact, in terms of smoking habits, on surgical outcomes? There are certainly opportunities for discussion throughout a patient’s surgical journey, from referral, initial consultation, through to pre-operative assessment. Given that smoking habits have such a significant impact on perioperative risk, it should surely also form part of the consent conversation? Too often, according to the evidence, these opportunities are missed. A large hospital based audit undertaken across the UK showed that 72% of patients were not asked if they would like to quit.
We need to open up these discussions. But how to do so, and do so effectively? Simply telling someone they should stop is unlikely to work.
Every day counts.
As well as thinking about how to have these conversations, we were also interested in the question of when. When should I stop smoking before surgery?
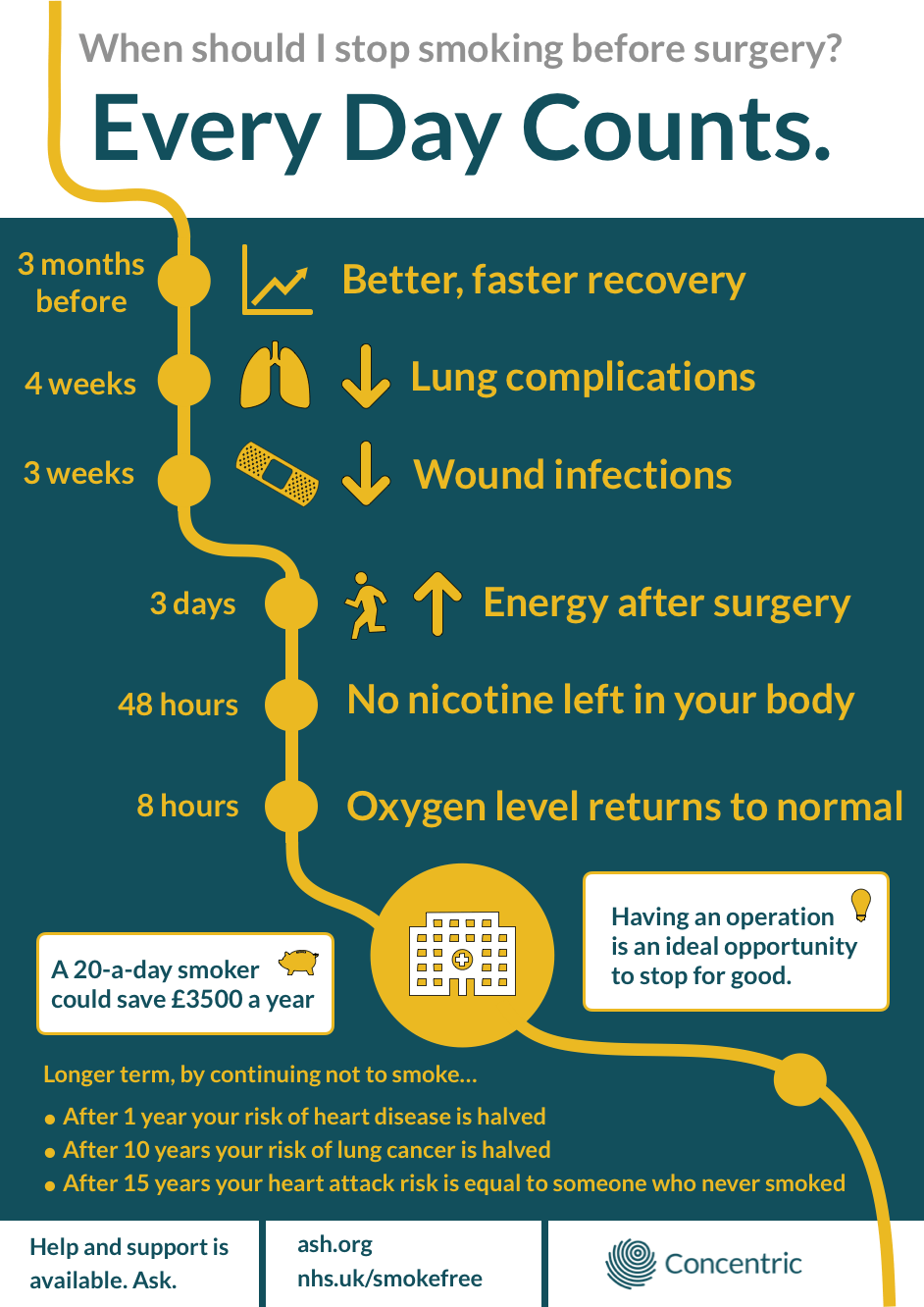
Studies have aimed to answer this question, and the evidence shows that varying periods of abstinence will reduce the risk of specific postoperative complications. Overall, quitting 3 months before surgery significantly improves a patient’s outcomes and reduces the smoking related risks.
But, if a patient misses the 3 month mark, then what? There is evidence that some pathophysiological changes caused by smoking return to near normal values in much shorter time frames. And this is very important. Smoking cessation for 3-4 weeks prior to surgery reduces the risk of respiratory complications and wound infections. Blood levels of carbon monoxide and nicotine - both cardiovascular stressors - fall to near normal within just 24-28 hours of stopping smoking, oxygen levels improve within 8 hours, and heart rate falls to normal in under one hour.
These changes impact on a patient’s risk of cardiovascular, respiratory and wound complications in their postoperative journey. It seems that ‘the earlier the better’, but ‘better late than never’ for stopping smoking before an operation. Fundamentally, it means that ‘Every Day Counts.’
In parallel to this blog, we’ve released an evidence summary, aimed at healthcare professionals, which summarises what is known about the effects of smoking on surgical outcomes.
An opportunity for change
Undergoing surgery is considered a ‘teachable moment’ for a patient. For most, it is a major life event. It is an opportunity for healthcare professionals to take a truly holistic approach. Patients may be more receptive to health and lifestyle advice at these times, and more motivated to make positive changes, to take control, including quitting smoking.
At Concentric, we appreciate the huge impact that open discussions can have for our patients, and are finding ways to incorporate them into everyday practice. Tailoring a risk discussion pre-surgery to the patient and their lifestyle is a key part of patient-centred medicine. Patients who smoke should be provided with information about their likely outcomes and the risks they face, to empower them to take the opportunity to make changes. These conversations improve our honesty and openness as a profession, and support our patients to make fully informed decisions about their health.
To support having conversations about stopping smoking at any point during the surgical journey, we’ve developed the below infographic - ‘Every Day Counts’. Feel free to make it available to your patients, and use it as a reminder to have the conversation.
In the past, in addition to public health campaigns to help and support quitting, multimodal interventions have been tried, including combinations of counselling, printed information, helpline referrals and nicotine replacement therapy. Some of these programs have been effective, but studies have been small, and interventions often represent an additional staff workload. It may not be achievable to replicate this widely.
However, in the age of digital health, there is an opportunity to reach out to our patients far more easily than we can put on additional preoperative consultations. Digital and video resources, as well as app based programs can be delivered to patients at home, in their own time. But the benefits go beyond convenience. These types of platforms are advocated by some to promote self motivation and empowerment better than didactic information given in a consultation room, and reduce the pressures of face-to-face counselling.
Quitgenius, a CBT based mobile app to aid smoking cessation has been very successful in supporting patients. 36% of users manage to stop smoking altogether, and of those who continue to smoke, the number of cigarettes smoked per day is reduced by 60%.
Conclusion
Smoking continues to be a significant contributor to adverse surgical outcomes. At Concentric, we want to equip clinicians and patients with tools to make positive health and lifestyle choices. We would advocate a realistic, united message that ‘Every Day Counts’ when it comes to the timing of smoking cessation preoperatively. Efforts to support this must be flexible and multimodal, focus on individual motivation and empowerment, and utilise increasing opportunities to use digital channels as an adjunct to traditional methods.
Let’s open the discussion. Let’s make Every Day Count.