Every Day Counts - Evidence Summary
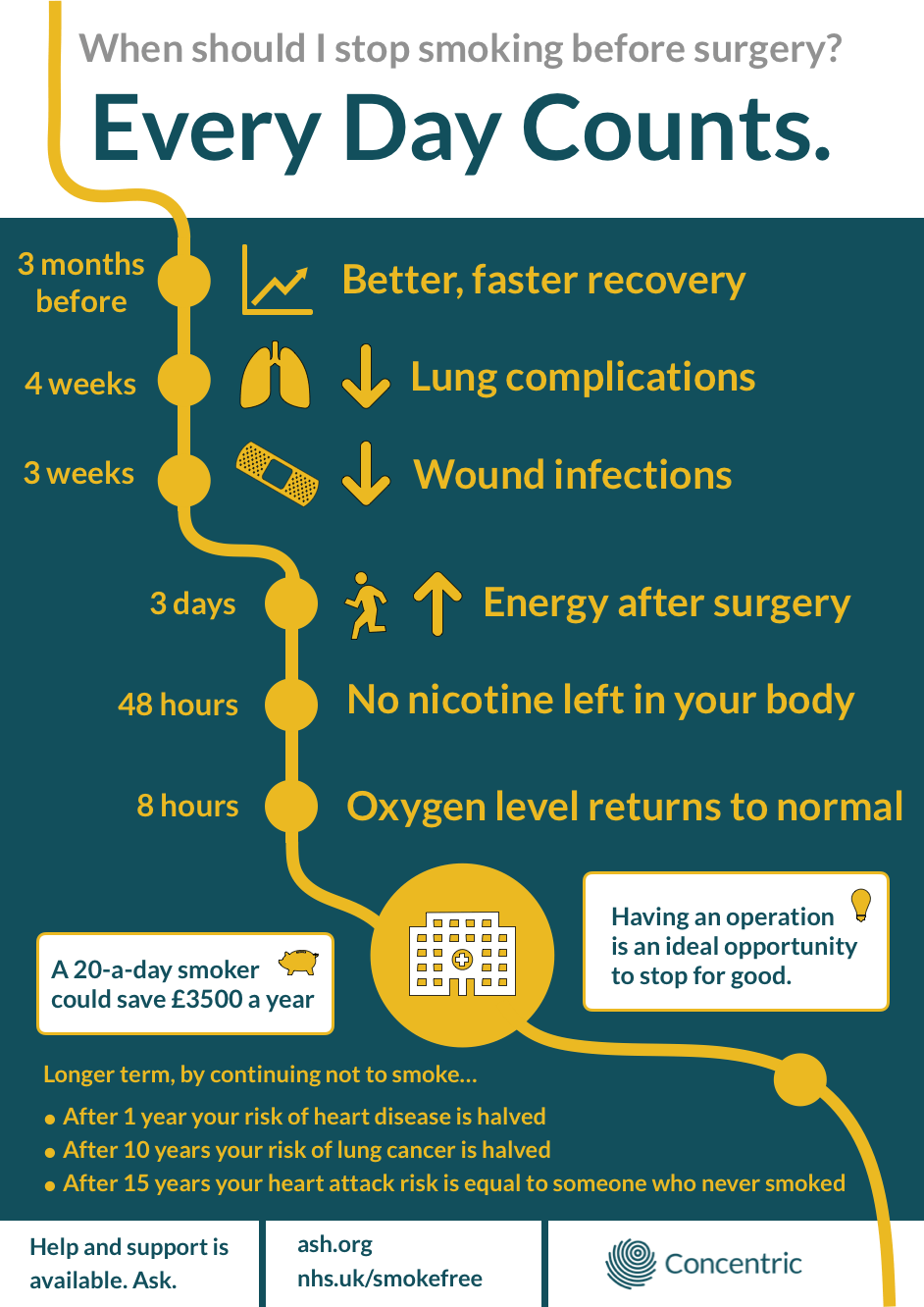
Every Day Counts is a series of resources - this evidence summary, an infographic and blog to examine the effect of smoking, and to support smoking cessation, in the perioperative period.
Healthcare professionals’ contact with patients during the surgical journey represents an opportunity for patient education, optimisation of comorbidities, and wider health promotion, including smoking cessation. Providing patients with accurate, tailored information aims to support and empower patients to make positive healthcare decisions to improve their outcomes from surgery, as well as their long term health.
In 2018, almost fifteen percent of the UK population smoked. While this represents a significant decline over the previous 40 years, it still amounts to 7.2 million people, and smoking continues to contribute to ninety-five thousand deaths a year.1 Twelve million operations and procedures are performed every year in the NHS,2 with smokers making up a significant proportion of this surgical population.
It is widely reported that smokers have an increased risk of adverse perioperative events, including; cardiac, pulmonary, and wound complications;3,4 increased admission rates to intensive care;5 longer hospital stays; and an increased risk of emergency readmission.6 Smokers are, on average, 38% more likely to die after surgery.4 They also have very real differences in self-perceived health when compared to non-smokers, being more likely to report having ‘very bad health’.1
Encouragingly, 58% of smokers over the age of 16 report a desire to quit.1 A period of hospitalisation for surgery is regarded as an opportunity to stop smoking. Beyond the simplicity of physically being in a non-smoking environment, patients in hospital have increased contact with healthcare professionals, more opportunities for discussion, information sharing and support. Patients may also be more receptive to consideration of their lifestyle choices, especially in the context of their impact on surgical risks. This opportunity, however, is scarcely utilised, with 72% of smokers not being asked whether they’d like to stop smoking, or be supported to do so, during their surgical journey.7
Effects of smoking on surgical outcomes, by system
Postoperative Pulmonary Complications
Postoperative pulmonary complications (PPC) describe any postoperative adverse event involving the respiratory system.8 These are common, and occur in part due to the changes that occur to the respiratory system during anaesthesia. General anaesthesia causes changes to respiratory drive, muscle function, lung volumes, ventilation-perfusion relationships, and causes a degree of atelectasis.8 Some of these changes also occur during neuraxial regional anaesthesia. Although common, the impact of PPC are not benign. They are associated with an increased length of hospital stay, increased morbidity, and 1 in 5 (14-30%) patients who have a postoperative pulmonary complication will die within 30 days of their operation. This compares to 0.2-3% of patients who do not have a PPC.8
With postoperative pulmonary complications having such a significant impact on the patient journey, it is useful to stratify the risk of PPC for an individual patient. Although clinical measurements such as spirometry, arterial blood gases and chest radiographs are not, in most cases, helpful in predicting individuals most at risk,8 studies have shown that smoking is a useful risk predictor for PPC in patients undergoing cardiac and non-cardiac surgery.3,4,9
Considering specific complications related to smoking, a study of data from 391,000 patients from the National Surgical Quality Improvement Program Database (NSQIP) showed that smoking status was independently associated with an increased risk of pneumonia (Odds Ratio 1.80, Confidence Interval 1.11, 2.92), unplanned intubation (OR 1.57, CI 1.10, 2.25) and requirement for ventilation for more than 48 hours (OR 1.73, CI 1.18, 2.53).4
Consideration of the pathophysiological changes that occur due to cigarette smoking helps to understand the increase in adverse events. Smokers have an increase in the volume and viscosity of secretions, which when coupled with ciliary dysfunction, leads to a loss of protective mucus clearance. Smokers often also have emphysema and loss of lung tissue elasticity, leading to an increased risk of pneumothorax during positive pressure ventilation. Airway obstruction seen in smokers also increases the chance of bronchospasm on induction of, and emergence from general anaesthesia.10
Cardiovascular Complications
Smoking increases cardiovascular risk in the perioperative period in two broad categories. The direct effect of being a current smoker, and via the increased risk of long-standing comorbidities.
Cigarette smoke contains over 5000 chemicals,11 many of which are harmful. Among them, with significant cardiovascular effects are nicotine and carbon monoxide. Nicotine stimulates the adrenal medulla to release adrenaline, and directly stimulates the sympathetic nervous system, resulting in increased heart rate, blood pressure, peripheral vascular resistance and myocardial contractility.10 These changes increase the oxygen demand of the myocardium. Carbon monoxide binds to haemoglobin with 250 times the affinity of oxygen,10 reducing available binding sites and therefore carrying capacity for oxygen. It also reduces the amount of oxygen delivered to the tissues, including the myocardium. The effect of increased oxygen demand coupled with reduced oxygen supply, particularly during the physiological stress of anaesthesia and surgery, results in significant risk of myocardial ischaemia, infarction and other cardiac events. This is supported by large patient data sets, showing that smokers have 57% increased risk of having a cardiac arrest in the 30 postoperative days, 80% increased risk of myocardial infarction, and 73% increased risk of stroke.4
Smoking also increases an individual’s perioperative risk via the comorbidities it contributes to. Smoking causes increased incidence of hypertension, coronary disease, atherosclerosis, peripheral vascular and cerebrovascular disease.12 Preoperative optimisation, or prehabilitation, is aimed at effective medical management of comorbidities, as well as promoting overall health and fitness measures, to minimise an individual’s perioperative risk.
Effect on Wound Healing
In addition to cardiopulmonary systemic effects, smoking has a negative impact on the healing of surgical wounds.13 The main predictor of wound healing is tissue oxygenation,14 and as previously explored carbon monoxide has a significant negative effect on tissue oxygen delivery. When tissue oxygenation is reduced, wound healing processes are impaired and there is an increased risk of wound breakdown and infection. Nicotine is also implicated, with evidence of vasoconstriction, increased platelet adhesion and attenuation of inflammatory processes, with implications for healing and ischaemic complications.14,15
This increased risk of wound complications in smokers has been demonstrated in a number of studies across surgical specialties.3,16,17 In particular, a meta analysis of 140 cohort studies including data from 478,000 patients found a statistically significant increase in wound healing complications in smokers compared to non-smokers, and in former smokers compared to those who had never smoked.17 This is supported by data from NSQIP, showing that in patients undergoing non-cardiac surgery, smoking confers a 30% increased risk of superficial and 42% increased risk of deep incisional infection.4 Again, these complications are not to be thought of lightly, with smokers having a 55% increased risk of developing septic shock following surgery.4 Similarly, in a study of patients who had undergone a hip or knee arthroscopy, in the group of patients who had required a hospital stay of longer than 15 days, the proportion of smokers who had wound complications was twice that of non-smokers.3
21st Century considerations
Electronic Cigarettes
When considering smoking behaviours in 2019, the use and impact of electronic cigarettes must be included. Newer to the market, these devices are mainly used by ex-smokers and current smokers to reduce tobacco consumption,18 and their use in these groups is promoted by the NHS.18,19 The prevalence of electronic cigarettes in the UK has risen sharply, being used by 3 million people in 2018.18
Less well studied than tobacco, patients using these devices represent an important group for clinicians to consider. These patients may not consider themselves smokers, and may be unaware that e-cigarettes - because they contain nicotine - can convey some harm, albeit significantly less harm than tobacco.18 Unless probed further into their smoking status and behaviours, any increase in risk due to e-cigarette use could go undetected.
This is demonstrated by a case report of a 51-year-old ASA-2 patient undergoing a bilateral mastectomy and reconstruction for cancer, who reported being a non-smoker preoperatively. The postoperative course was complicated by extensive flap necrosis requiring further returns to theatre. When questioned later, the patient revealed that she had been extensively using an e-cigarette right up to the time of surgery.20 While the e-cigarette use cannot be regarded as causal in her complications, this case demonstrates a common scenario in clinical practice, where the clinician and patient use different language, make different assumptions, and label certain behaviours differently. These difficulties can lead to misunderstandings and difficulties in conveying individual risk information.
The use of these devices may also be far more difficult to quantify than tobacco cigarettes, due to different strengths of the nicotine-containing vapour marketed (maximum strength 20mg/ml in the UK21), and the ease of more continuous use rather than discrete smoking episodes. This demonstrates the need for clinicians to precisely discuss and explore with patients any behaviours that may influence their perioperative risk.
Preoperative smoking cessation interventions
Less well appreciated than the increase in perioperative risk due to smoking is the optimal timescale for preoperative cessation in order to convey benefit. A number of studies have aimed to estimate this, suggesting a period of abstinence of at least 3 weeks to reduce complications related to wound healing,22,23 4-8 weeks to reduce respiratory complications,23,24 and 90 days to reduce overall morbidity.25
Ways to achieve preoperative smoking cessation have also been evaluated. Multimodal intervention, including combinations of counselling, printed information, helpline referral and nicotine replacement therapy, commenced at the time of pre-assessment, has been shown to be effective at reducing smoking rates on admission and at 30 days postoperatively.26 However, these studies are small and therefore subject to a number of biases. Interventions described have often also represented a change or addition to the pre-assessment clinic workload, something that may not be widely achievable or sustainable across multiple healthcare settings and patient groups.
In addition, we need to consider a heterogenous group of patients and healthcare journeys. A period of weeks or months abstinence from cigarette smoking may convey the greatest health benefits, but this is not always practical or possible. Even a period of hours of abstinence will reverse some of the detrimental effects of nicotine and carbon monoxide (see table). For example, after 48 hours, nicotine, the addictive component of tobacco, is eliminated from the body. Achieving an initial period of abstinence may spur ongoing motivation to continue a smoking cessation journey in the long term. A realistic, united message to patients should therefore perhaps be that any achievable period of abstinence before surgery will offer benefits.
Clinicians also have a good opportunity to reinforce the benefits of smoking cessation during the postoperative inpatient recovery period, and to go on to discuss the long term health, social and financial benefits of not smoking, whether a patient stopped prior to surgery or not.
In the age of digital health, is the best way to support patients to stop smoking changing? Are there opportunities to more efficiently target information sharing, or to better empower patients to make positive changes in the perioperative period? There is evidence that goal setting and psychological empowerment provided by targeted mobile health apps can help over a third of users to successfully quit, with those still smoking also smoking significantly less per day.27
Every Day Counts infographic
Conclusion
As clinicians, we have a unique opportunity to help our patients to make positive informed decisions, not just relating to their planned surgery but also to their wider health and lifestyle. We can best support by understanding motivations, discussing accurate and understandable information, and providing usable, flexible interventions.
The evidence reviewed regarding smoking in the perioperative period demonstrates that there is still more to do to support smoking cessation efforts, with smoking continuing to be a significant contributor to poor surgical outcomes.
The authors, following review of the evidence, advocate a realistic, united message that ‘Every Day Counts’ when it comes to timing of smoking cessation preoperatively. Efforts to support smoking cessation should be flexible and multimodal, and should utilise increasing opportunities to use digital channels as a significant adjunct to traditional methods.
Pathophysiological impacts of smoking cessation at different time-points post cessation. 10,28
| Timeframe | Effect |
|---|---|
| After 20 minutes | Heart rate returns to normal. |
| After 8 hours | Blood nicotine and carbon monoxide levels reduced by more than half. Oxygen levels return to normal. |
| After 48 hours | Carbon monoxide eliminated from the body. Lung mucus clearance improves (improved ciliary function). Nicotine is cleared from the body. Taste and smell start to improve. |
| After 72 hours | Airway obstruction starts to improve. Energy levels increase. |
| After 2 weeks | Sputum volume returns to normal levels. |
| After 2-12 weeks | Circulation improves. |
| After 3-9 months | Tracheobronchial clearance improves. Lung function increases by up to 10%. Cough, wheeze and shortness of breath improve. |
| After 1 year | Risk of heart disease is around half of that of a smoker. |
| After 10 years | Risk of lung cancer falls to half that of a smoker. |
| After 15 years | Risk of heart attack falls to the same as someone who has never smoked. |
References
1 - Adult smoking habits in the UK: 2018. Office of National Statistics
2 - Hospital Admitted Patient Care Activity 2017-18. NHS Digital
6 - NICE Guidelines (PH48) Smoking: acute, maternity and mental health services. 2013
10 - Thiagarajan N. Smoking and Anaesthesia. Anaesthesia Tutorial of the Week. 221. 2011
12 - Smoking and cardiovascular disease. Centers for Disease Control and Prevention
13 - The Clinical Case for Smoking Cessation before Surgery. Interventions in Secondary Care. NHS
15 - Silverstein P. Smoking and wound healing. Americal Journal of Medicine. 1992;93(1A):22S-24S
18 - Action on Smoking and Health. Use of e-cigarettes (vapourisers) among adults in Great Britain. 2018
- 21 - All you need to know about vaping. Vape UK