Earlier this year, Health Innovation Oxford & Thames Valley (HIOTV), part of the UK’s Health Innovation Network, published an independent impact assessment of Concentric’s implementation across two NHS Trusts within the Buckinghamshire, Oxfordshire and Berkshire West Integrated Care System (BOB ICS).
As we reach the 50% milestone of UK NHS Trusts adopting or beginning to implement digital consent, it is a good opportunity to critically review the report in detail. My goal is to understand the new insights it offers regarding Concentric’s impact and identify important questions that warrant further exploration. You can read more about the existing published evidence in our digital consent research overview page.
Who and why
Through NHS England’s Health Technology Adoption and Acceleration Fund (HTAAF), the BOB ICS, including Oxford University Hospitals (OUH) and Buckinghamshire Healthcare (BHT), received funding to support the rollout of Concentric.
As part of that programme, the BOB ICS commissioned HIOTV to evaluate the early impact of Concentric’s deployment in Ophthalmology at OUH and Obstetrics & Gynaecology at BHT. The evaluation combined two elements: stakeholder engagement with healthcare professionals and a preliminary health economic analysis comparing paper and digital consent pathways at both Trusts.
Methodology
Stakeholder engagement
At OUH, HIOTV ran a focus group with 11 ophthalmology clinicians. At BHT, they conducted one-to-one interviews via Microsoft Teams with Obstetrics & Gynaecology staff. The report lists five job roles, but does not specify how many participants there were.
Across both sites, discussions followed a structured guide that explored ease of use, efficiency, data reliability, consent-related issues, and shared decision-making (appendices 1 and 2 of the report).
Health economic analysis
The researchers first conducted a literature review to identify the “critical parameters” for evaluating paper-based and digital consent pathways. These align with how we already think about, and communicate, the potential impact of digital consent:
- Time savings and associated economic benefits
- Rates of missed or incomplete forms
- Frequency of day-of-surgery delays or cancellations, and their associated costs
- Potential reduction in medicolegal claims and related costs
At OUH, the team then used a structured data collection tool to gather data on implementation and ongoing costs, consent volumes, staff time, rate of consent-related issues, operational efficiencies and delays, and medicolegal claims (Appendix 6). Aside from the per-episode analysis, two time horizons were applied: an eight-month view (reflecting the duration of Concentric’s use at OUH) and a three-year view (based on the average lifespan of iPads and expected staff retention).
Due to the lack of data from BHT, a hypothetical analysis was conducted using existing literature, which was neither interrogated nor extended. As such, while it may be a helpful reference point for Trusts of a similar size, this analysis does not add new insight and is not explored further in the findings.
Findings
💬 Patient experience
The report asserts that digital consent enhances shared decision-making and improves patient satisfaction, which is consistent with previous studies. It is worth noting, however, that no patients were interviewed, so these findings reflect clinician perceptions rather than patient-reported experience.
At OUH, clinicians “all agreed” that patients had “no issues” with using digital consent and described positive signing experiences, including comparisons to “signing for a parcel”. While encouraging, we know from existing patient feedback that challenges do exist, and this gap highlights why direct patient input is essential during evaluation. There is also more to understand about the nuance of patient experience, including differences between in-person and remote consent, and how digital access, confidence, and comprehension vary across patient demographics.
As part of his elective placement with us, medical student Dunsin Oderinlo recently undertook a project to begin systematically analysing our large dataset of patient feedback to explore these patterns. We encourage Trusts to undertake similar analyses or to engage patients directly to understand how digital consent impacts shared decision-making and patient experience.
🧑⚕️ Staff experience
The evaluation provides some of the first structured clinician feedback we have seen, with most insights until now coming through informal channels or in-app feedback. Perhaps unsurprisingly, BHT’s one-to-one interviews produced more granular and, at times, more critical reflections, likely because individuals felt more able to speak candidly in a one-to-one setting.
Even so, no new themes emerged, and the positives described across both Trusts echo what we have heard before: efficiency gains, ease of use and navigation, reduced risk of errors, and the benefits of being able to share consent information with patients.
Approaches to rollout and training vary widely across deployments. Although we don’t prescribe a single method, we consistently see certain practices in successful rollouts: an active project team, open communication, sustained engagement with clinical teams, and visible clinical champions. Despite different approaches (OUH used one-to-one training, and BHT used group training with additional sessions as needed and now mandatory e-learning), clinicians in both organisations highlighted these same factors as positive parts of their experience.
In terms of data security and reliability, clinicians had confidence in their Trusts’ cybersecurity processes and no unique concerns specific to Concentric. They also described an increased sense of security and governance benefit, linked to fewer lost forms and improved traceability and auditability. Although we often frame medicolegal benefit in terms of potential cost savings, this everyday confidence is valuable in its own right. BHT clinicians raised the specific issue of data security on shared devices, particularly when users did not log out properly. Although they attributed this to human error, it highlights a genuine challenge in determining appropriate inactivity timeouts in clinical environments. Longer timeouts may be acceptable on personal devices, which already provide inherent security protections, whereas on shared devices, shorter timeouts are required to provide the appropriate privacy assurances.
⏱️ Clinical efficiency
Clinicians at OUH and BHT all agreed that adopting Concentric had positively impacted clinical efficiency by reducing administrative time during the consent process, making amendments easier, and reducing errors and incomplete forms.
Quantifying perceived efficiency gains can be difficult. For OUH’s economic analysis, the consent process was broken down into individual clinical and administrative tasks. With the time spent explaining consent unchanged (10 minutes), the savings from digital consent came mainly from locating and completing consent forms more quickly and from no longer having to scan, store, or dispose of paper forms.
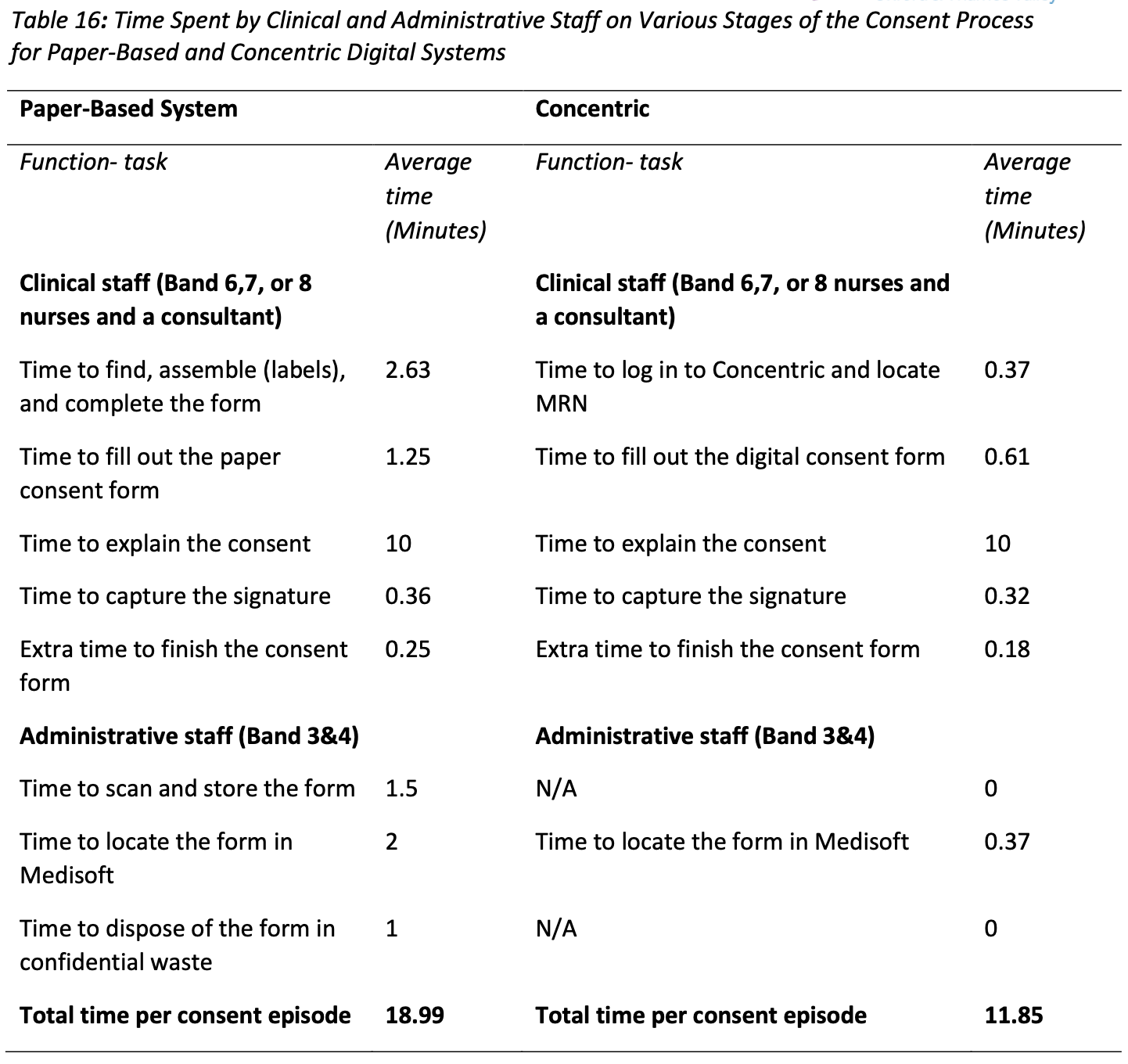
This granular approach offers a practical way to quantify time savings, though the methodology for deriving time estimates for each task is not described.
There is nuance around the true financial significance of the time saving, and the report does not explore whether some, all, or none of the time saving was likely to be cost-releasing in the short or medium term. There is, however, an engaging narrative around the potential impact on operational flow and patient throughput. Staff in OUH’s eye injection clinics reported that faster consent confirmation enabled them to accommodate more urgent or on-the-day cases. The report does not quantify this effect, but it would be worth exploring further to fully understand and consider how efficiency gains could be replicated in other high-volume services.
💰 Cost savings
The total cost per consent episode ranged from £7.48 to £25.18 for the paper-based process and from £5.51 to £19.54 for the Concentric process, depending on whether a minimum-cost (using nursing salary bands) or maximum-cost (using consultant salary rates) scenario was applied. The headline saving of £5.64 per consent episode (equating to around £850,000 for an average-sized NHS Trust over three years) was based on the maximum-cost scenario, which therefore almost certainly overstates the actual savings. Still, even the lower-bound scenario shows a clear cost advantage for digital.
Looking at the underlying breakdown of cost per episode – split into process costs (materials and disposal for paper; infrastructure, training and licensing for digital) and staff time – it becomes clear that most of the savings, in this analysis, come from the seven minutes of staff time saved per episode.
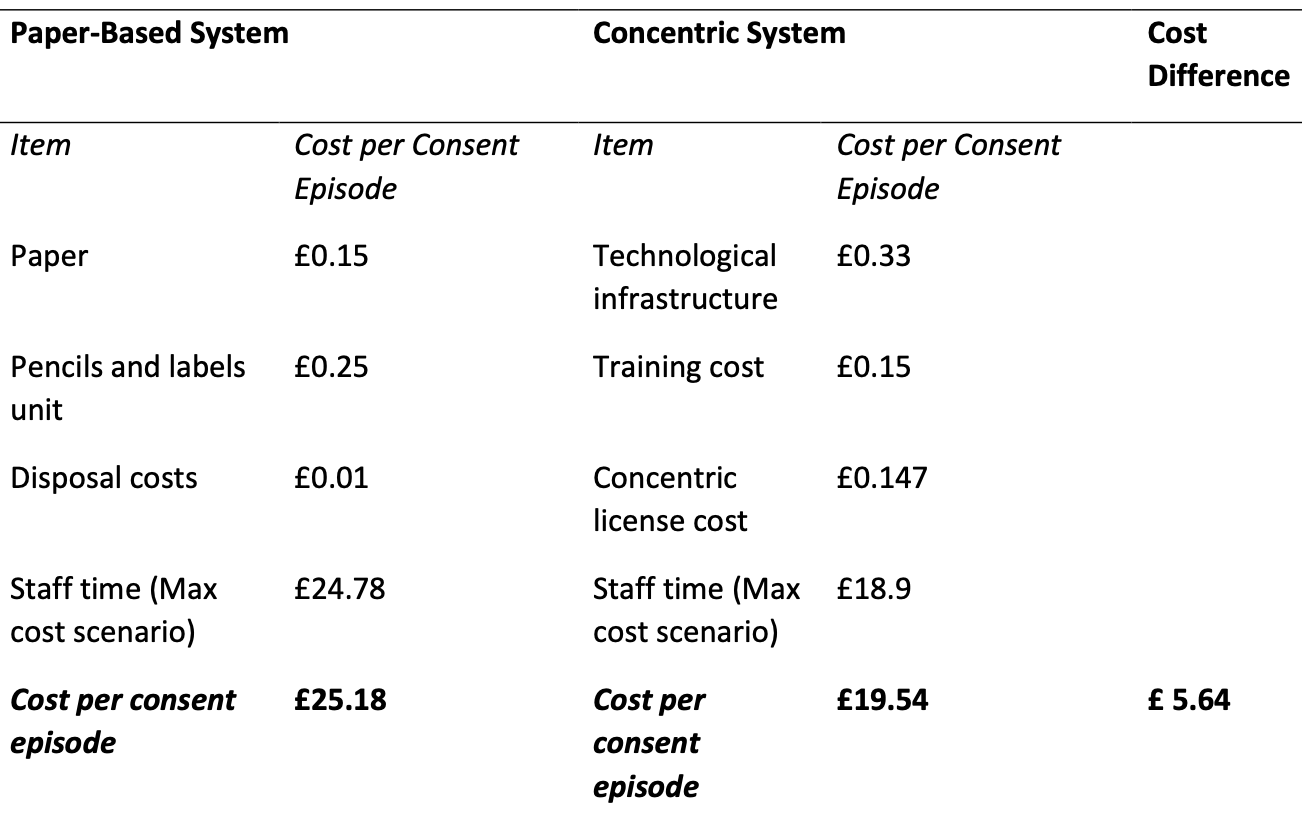
However, unlike staff time, process costs are cash-releasing and seeing them side by side is helpful. As more pathways are digitised, the cost of maintaining small pockets of paper tends to rise, something that may be overlooked when building a business case for digital consent. OUH’s three-year horizon (representing average iPad lifespan and staff retention) also offers a practical way to think about these costs over time.
The evaluation also explored other potential sources of cost saving:
- Missed forms: OUH internal audit data showed a 1.95% lost consent form rate with paper, a figure eliminated with Concentric. The projected saving assumes Consultant-led re-consenting and may therefore be overstated. Still, the underlying approach (identifying and quantifying the local rate of lost forms and the process implications) may be a valuable exercise for organisations considering digital consent.
- Delays: Four day-of-treatment delays occurred with the paper process, compared to none with Concentric, broadly aligning with existing evidence of a 5-10% reduction in day-of-surgery delays with digital consent. However, attributing delays directly to consent is challenging, and more work is needed to measure this impact robustly. We also haven’t seen this explored in a business-as-usual setting, where we might expect the pattern to differ from an active deployment.
- Medicolegal: Every year, 12,000 medicolegal claims are brought against the NHS in England, at a cost of £8 billion. Consent-related claims are a notable subset and include “failure to warn” (where patients report not being informed of significant risks a reasonable person would want to know), inadequate explanation of alternatives, poor communication and incomplete documentation. Previous work with medicolegal teams has estimated that Concentric reduces the failure-to-warn risk by 50%. During the evaluation period, no consent-related claims were recorded with Concentric. While the timeframe is too short to draw firm conclusions (a limitation the authors also acknowledge), if this pattern continues, the potential cost savings are substantial.
Final thoughts
HIOTV’s evaluation adds meaningful weight to the case for digital consent, strengthening the existing evidence in places and giving greater credibility to the anecdotal benefits we hear day to day. Improvements in efficiency, documentation quality, medicolegal assurance, and both realised and project cost savings are clear, alongside several areas warranting further exploration.
From an evaluation perspective, the report also offers a pragmatic blueprint for assessing some of the more challenging aspects of digital transformation, including efficiency gains and cost-per-episode savings. While some methodological details are missing, the overall approach may serve as a helpful starting point for organisations looking to assess the impact of digital consent in a structured, locally meaningful way.
As services continue to scale the use of digital consent, direct patient insight, more robust approaches to measuring delays and throughput, and longer-term tracking of medicolegal trends will be key to building a richer, more complete understanding of its impact.
“This report showed that Concentric’s digital consent tool could bring big benefits to patients, improve safety and increase productivity if adopted more widely across the NHS”
- Guy Checketts, Head of Transformation and Evaluation at HIOTV
Read the full HIOTV report here
